What is thalidomide and what caused the thalidomide disaster of the 1950s and 60s?
Thalidomide was first developed by Chemie-Grunenthal, a German pharmaceutical company, in 1954. It was first marketed as a sedative, and was far more effective that the alternative of the time – barbiturates. It was non-addictive, didn’t give rise to tolerance and didn’t depress respiration. Soon after its release onto the market it was discovered to be an effective anti-emetic (preventing vomiting) and was used to treat morning sickness which usually occurs in the first trimester of pregnancy (during the period of organogenesis). The drug soon became widespread (46 countries) and was widely marketed and advertised as a safe drug.
It was only in the early 1960s that reports started to come in detailing occurrences of severe birth defects, ‘flipper-like limbs’, with a significant increase in phocomelia (shortening of the limbs) and amelia (no limbs). The increase in defects was only related to the drug because these conditions are exceptionally rare in humans (only 1 in 4 million births). In 1961, Lenz in Germany and McBride in Australia confirmed thalidomide to be the cause of these teratogenic effects. This was the biggest man made medical catastrophe with 10,000 severe birth defects in children, and about 5,000 of these survived to adulthood. It is not known how many babies died in utero but a marked increase in miscarriages and stillbirths was seen in this period with estimates over 100,000 additional ‘deaths’. Thalidomide was withdrawn from the market in the UK in November 1961.
Dr Frances Kelsey of the FDA was responsible for licensing drugs in the USA at this time, but she was concerned about the safety of the drug due to a side effect – peripheral neuropathy which causes numbness and tingling in the hands and feet. She also feared about the effects on pregnancy so didn’t licence the drug for use in the USA. This averted the disaster occurring in the USA and she was given the Presidents Award for Distinguished Federal Civilian Service.
Very few organs in the body weren’t affected in some way by thalidomide. Most commonly in the limbs but also seen was significant damage to the face, eyes, ears, genitalia, heart, kidney and gastrointestinal tract. The exceptionally high infant mortality is attributed to internal organ damage.
The mechanism of action of thalidomide is unknown – although this is still being studied and a credible reaction cascade has been proposed from various hypotheses. Thalidomide (also known as alpha-N-phthalimidoglutarimide) exists in 2 forms. It has a chiral carbon which means it can exist in 2 enantiomers an R-enantiomer and an S-enantiomer.

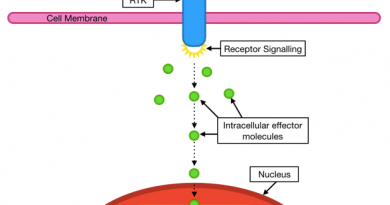
The S-enantiomer is thought to be teratogenic, and the R-enantiomer is thought to provide the sedative effect, but it is very hard to stabilise this switching as it occurs in any aqueous environment (e.g. cellular) and doesn’t require enzymes to catalyse it. The drug given to patients was a racemic mix of both enantiomers. This was further broken down into 18 metabolites with various molecular targets (Cereblon, tubulin and nitric oxide), however the exact molecular effects and mechanisms are not fully understood.
The thalidomide disaster was a tragedy, but some good came out if it in the pharmaceutical industry. Partly as a result of this disaster drugs are now tested far more extensively than they were in the 1950s and 60s, and there has not been a repeat of the disaster. Drugs are tested using rabbits as they are more sensitive to teratogenic effects than mice and are useful in analysing whether a drug causes birth defects.